Introduction:
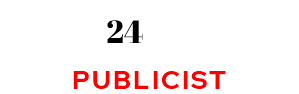
The Pressure of Labor Costs on Healthcare
Rising labor costs have become one of the most pressing challenges for healthcare leaders across the globe. With the lingering effects of the COVID-19 pandemic, an aging population, and soaring inflation, hospitals and clinics are under more financial strain than ever before. Healthcare systems must now rethink how they recruit, retain, and manage their workforce while maintaining quality care.
Labor, often accounting for 50-60% of a hospital’s operating budget, is not just a cost—it’s the foundation of healthcare delivery. So how are industry leaders adapting to ensure sustainability and growth? In this article, we explore 7 powerful strategies that are reshaping healthcare labor management in 2025 and beyond.
Why Labor Costs Are Surging in Healthcare
The Role of Inflation
Inflation has touched every sector, and healthcare is no exception. Rising wages for nurses, physicians, and support staff are driven by survey, commissioned by healthcare staffing platform Nursa general inflation, but also by increased bargaining power of workers post-pandemic. Cost-of-living adjustments are becoming standard, adding pressure to already-tight budgets.
Workforce Shortages Post-Pandemic
The pandemic accelerated burnout and retirement among healthcare workers. Many professionals left the industry, creating a gap that new graduates can’t fill fast enough. As demand exceeds supply, labor becomes more expensive.
Increased Demand for Specialized Care
An aging population and chronic disease prevalence require more complex and continuous care. Specialists, such as nurse practitioners, respiratory therapists, and behavioral health professionals, are in higher demand—pushing salaries upward.
Strategy 1:
Investing in Workforce Retention Programs
Retaining existing staff is more cost-effective than hiring new employees. Healthcare leaders are recognizing that happy employees are more productive and less likely to leave.
Benefits Packages and Incentives
Offering competitive compensation is essential, but it doesn’t stop there. Comprehensive benefits such as:
- Tuition reimbursement
- Loan forgiveness programs
- Mental health support
- Housing stipends
have become critical in keeping healthcare workers satisfied.
Flexible Scheduling and Remote Opportunities
Healthcare jobs—especially in administration and telehealth—are becoming more flexible. Leaders are providing remote options and flexible hours, which reduce burnout and increase job satisfaction.
Strategy 2: Leveraging Automation and AI Technologies
Technology isn’t replacing clinicians—it’s supporting them. Automation reduces administrative burden, allowing clinical staff to focus on patient care.
Streamlining Administrative Tasks
Tasks like scheduling, billing, and documentation are increasingly handled by AI-powered platforms. This lowers the need for clerical staff and reduces overtime hours.
Enhancing Clinical Decision-Making
AI tools are improving diagnostics and treatment planning, saving time and improving outcomes. For example, IBM Watson and similar platforms analyze patient data to assist physicians in making faster, evidence-based decisions.
Strategy 3: Upskilling and Cross-Training Staff
Instead of hiring for every skill gap, hospitals are upskilling their current staff.
Building a More Versatile Workforce
Nurses are being trained in IT systems, and lab technicians are learning patient engagement skills. This cross-functionality reduces the need for multiple roles, saving money.
Reducing Dependency on New Hires
Training programs allow organizations to grow talent from within, which is cheaper and more reliable than external hiring.
Strategy 4: Restructuring Labor Models
Modern healthcare requires flexible, adaptive staffing models.
Outsourcing and Telehealth Integration
Administrative roles, customer service, and even virtual health consultations are being outsourced to specialized firms or remote teams—offering quality service at lower costs.
Collaborative Staffing Models
Hospitals are partnering with regional systems to share staff during surges, like flu season or pandemics, reducing the need for temporary hires.
Strategy 5: Emphasizing Value-Based Care Models
Shifting from fee-for-service to value-based care helps manage costs while improving quality.
Aligning Incentives with Outcomes
Providers are rewarded for keeping patients healthy rather than performing more procedures. This reduces unnecessary work and lowers labor demand per patient.
Lowering Costs Without Compromising Quality
Hospitals that embrace value-based models report lower readmission rates, better outcomes, and more satisfied staff due to clearer roles and expectations.
Strategy 6: Strategic Use of Contract Workers
Many healthcare systems are turning to contract workers to address fluctuating labor demands while controlling long-term costs.
Temporary Staffing Solutions
Travel nurses, locum tenens physicians, and per diem workers are now key parts of healthcare staffing models. These professionals help fill urgent gaps, such as during seasonal demand spikes or pandemics, without the 60 percent of hospitals’ total expenses need for permanent hires.
However, leaders must balance these benefits with potential downsides—such as higher hourly rates and less continuity in patient care.
Balancing Full-Time vs Per Diem Staff
A strategic mix of full-time, part-time, and contract labor enables more flexible staffing while safeguarding continuity. Leaders are now using predictive analytics to determine the optimal ratio, allowing them to:
- Reduce overtime
- Minimize burnout
- Cut avoidable expenses
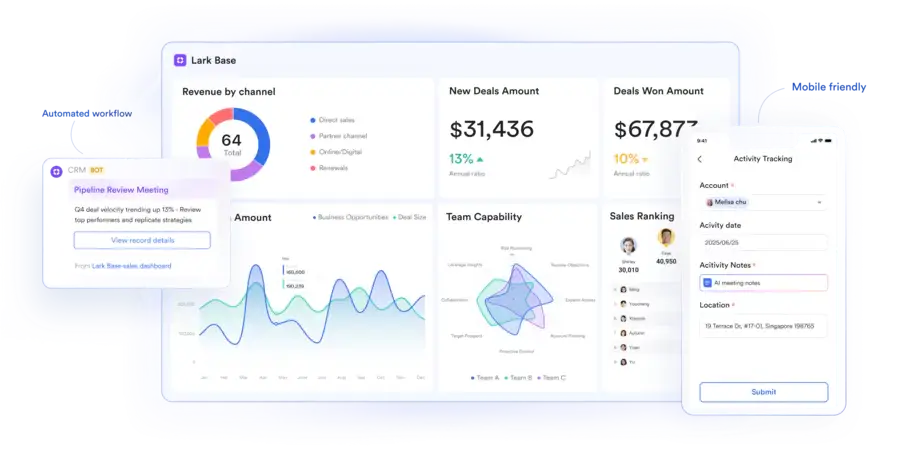
Strategy 7: Data-Driven Labor Management
Healthcare leaders are embracing data analytics to make informed staffing decisions and proactively manage costs.
Real-Time Analytics in Workforce Planning
Sophisticated platforms now allow real-time insights into staffing levels, patient acuity, and operational costs. By aligning labor resources with patient needs, systems avoid both overstaffing and understaffing.
For example, solutions like Kronos Workforce Analytics or Oracle Health help facilities:
- Forecast shift demand
- Track overtime patterns
- Monitor staff utilization
Forecasting Budget and Staffing Needs
Budgeting based on historical data often leads to inefficiencies. Instead, modern workforce planning tools use AI and trend analysis to forecast future staffing needs, allowing timely adjustments and better financial management.
The Role of Healthcare Leadership in Navigating Change
Adapting to rising labor costs isn’t just a numbers game—it requires strategic leadership and organizational culture shifts.
Fostering a Culture of Innovation
Leaders must create environments where staff are encouraged to embrace change. This includes:
- Implementing pilot programs for new labor models
- Supporting interdisciplinary collaboration
- Recognizing and rewarding innovation
Innovation is no longer a luxury—it’s a necessity.
Transparent Communication with Staff
Transparent communication builds trust and encourages employee buy-in. Leaders must regularly communicate:
- The reasoning behind staffing decisions
- Organizational goals and cost challenges
- Opportunities for staff development
Engaged and informed staff are more likely to stay and contribute positively to the organization.
Challenges Ahead: Regulatory and Ethical Considerations
While innovation is crucial, it must be balanced with ethical responsibility and regulatory compliance.
Compliance with Labor Laws
As healthcare organizations adjust labor models, they must ensure compliance with federal and state labor laws, such as:
- Minimum wage requirements
- Overtime regulations
- Fair labor standards
Violations can lead to hefty fines and reputational damage.
Ethical Staffing Practices
Decisions about layoffs, automation, or outsourcing must be made with compassion and ethics in mind. Patient care should remain the top priority, and workers must be treated fairly during organizational transitions.
FAQs
1. Why are healthcare labor costs increasing so rapidly?
Labor costs are rising due to inflation, staff shortages, higher demand for specialized care, and post-pandemic workforce shifts.
2. How can healthcare organizations retain staff effectively?
Retention strategies include offering competitive benefits, flexible work schedules, mental health support, and professional development opportunities.
3. Is automation replacing healthcare workers?
No, automation supports rather than replaces clinical roles. It helps reduce administrative burdens and streamline care delivery.
4. What is value-based care and how does it affect labor costs?
Value-based care ties compensation to patient outcomes rather than services rendered. It helps reduce redundant labor while maintaining high-quality care.
5. Are contract workers a sustainable solution?
They are effective short-term solutions but can be costly long-term. A balanced staffing model is crucial for sustainability.
6. How does data help in managing labor costs?
Real-time data helps predict staffing needs, optimize schedules, reduce overtime, and align labor with patient demand.
Conclusion: Building a Resilient Healthcare Workforce
Rising labor costs in healthcare are undeniable—but they are not insurmountable. Leaders who adopt innovative, data-driven, and employee-focused strategies are not just surviving—they’re thriving.
By focusing on workforce retention, embracing technology, and reimagining labor models, healthcare organizations can maintain both quality care and financial stability. The future of healthcare staffing is agile, intelligent, and deeply human-centered.